
A Guide To Repairing Family Relationships
Discover expert tips for repairing family relationships and fostering healthy connections with The Recovery Team.
At The Recovery Team, we can help you get your life back on track. We offer a range of care options for drug and alcohol abuse and behavioral addiction. Our experts can guide you through inpatient, residential, and outpatient programs tailored to your needs and preferences. All therapies, programs, and treatments are designed with your individual situation in mind.
Most insurance accepted
![]()
![]()
![]()
![]()
![]()

Addiction to alcohol, drugs, and certain behaviors can be difficult for everyone—from family members and spouses to employers and entire communities. However, there is hope: treatment options are available to help you recover from any substance. Don’t give up now!

Sedative hypnotics are prescription drugs used as sleeping pills or sedatives that affect your central nervous system and have a calming effect on your body. Older adults with anxiety or insomnia commonly use sedative drugs.
Further Info
Opioid addiction is common among Americans due, in part, to the Ove prescription of opioid pain relievers. Moreover, opioid abuse leads to opioid use disorder, and more than 2.5 million Americans have faced the condition of opioid use disorder.
Further Info
In 2020, more than 28 million people over 12 met the criteria of alcohol use disorder. Alcohol treatment can reduce harm caused by AUD
Further Info
Tailoring treatment approaches to the individual is essential for successful addiction recovery. Every person is different, so what works for one may not be good for another. Taking the time to get to know each client, understand their individual needs and circumstances, and develop a plan that is tailored to them increases our chances of giving you lasting recovery.
At The Recovery Team, we focus on providing personalized care. Our team of experienced professionals give the time and attention patients need to feel better. We look at the whole picture and develop an individualized treatment plan that is made for your needs and goals. We believe in using only evidence-based treatments that researchers have proven to be highly effective.
Transcranial Magnetic Stimulation (TMS) Therapy is a non-invasive treatment for depression and other mental health disorders. TMS is useful for those who have not had success with other forms of therapy or medication
Eye Movement Desensitization and Reprocessing (EMDR) is a type of psychotherapy that helps people process and heal from traumatic experiences. It can reduce the intensity of negative emotions and beliefs
Cognitive Behavioral Therapy is psychotherapy that works to address negative thought patterns and behaviors that can contribute to mental health issues. It creates healthier ways of feeling, thinking, and acting

Delray Beach, FL
Find top-notch therapy and recovery in beautiful Delray Beach at our second South Florida location. We offer residential care, and aftercare services.

Contact
When you call The Recovery Team, a member of our team will work with you on the phone to do a pre admission assessment. This assessment takes 15 to 30 minutes and is a clinical evaluation of your drug and alcohol use, as well as any mental health problems like anxiety, depression, or mood disorders.
Review
To speed up the admissions process, we’ll collect your insurance and financial information during the initial assessment, if applicable. After verifying your insurance benefits, a member of our team will explain your co-pays and payment options, and then determine if our facility is the right fit for your individual needs.
Arrival
Generally, we bring clients to our facility within 24 hours of the pre-admission assessment, provided all criteria have been assessed and met. During this time, our team will stay in touch with you to ensure your safety and arrival

A Guide To Repairing Family Relationships
Discover expert tips for repairing family relationships and fostering healthy connections with The Recovery Team.

How To Set Boundaries With People: A Practical Guide
Discover practical tips on how to set boundaries with people in this expert guide from The Recovery Team.
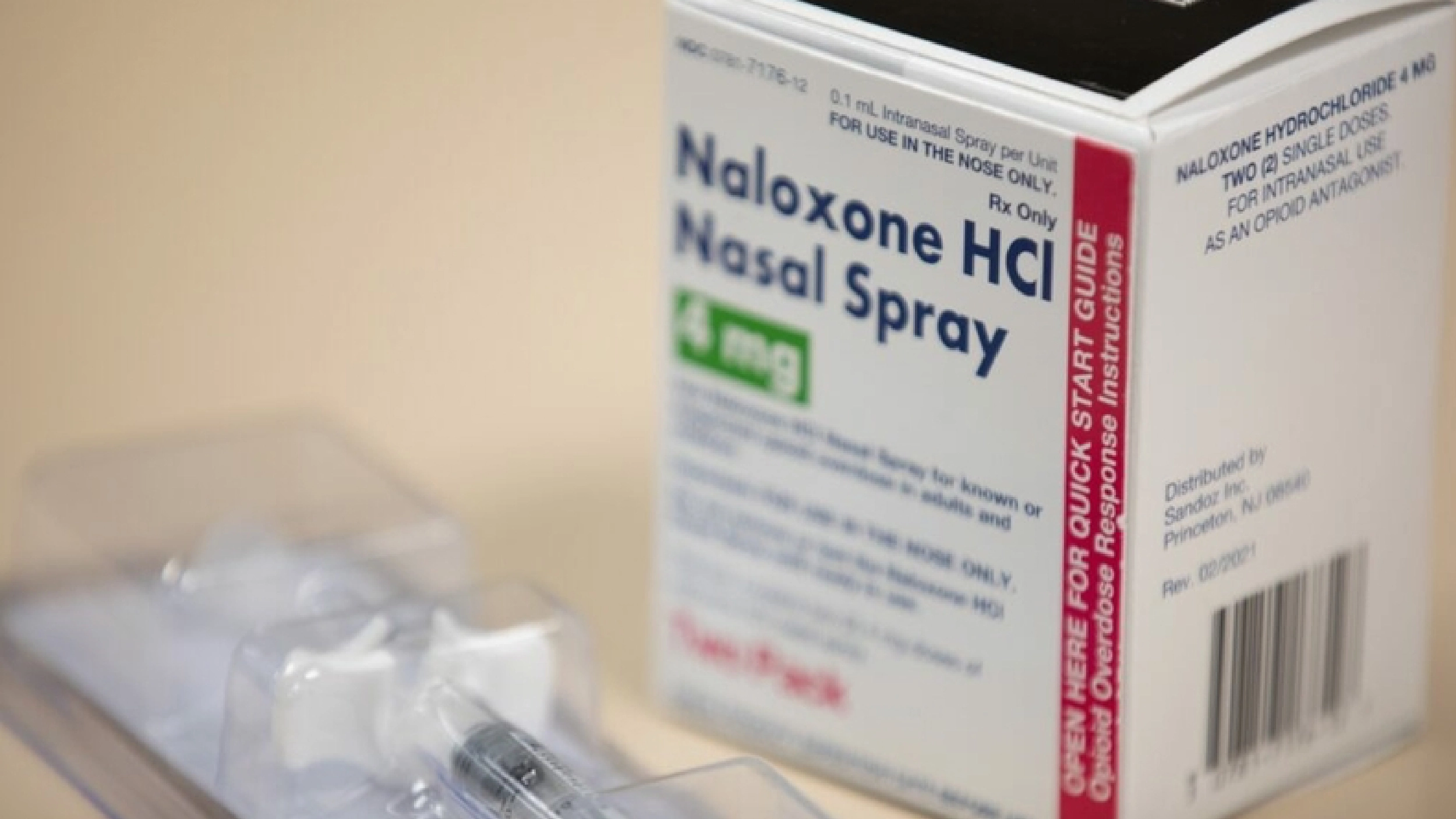
Administering Naloxone: Be Prepared, Save a Life
Naloxone saves lives. The Recovery Team shares how to reverse an opioid overdose with this drug.