
A Guide To Repairing Family Relationships
Discover expert tips for repairing family relationships and fostering healthy connections with The Recovery Team.

Seasonal affective disorder (SAD) is a subtype of depression characterized by recurrent depressive episodes that align with specific seasons, most commonly during fall and winter.
The condition’s onset is thought to be linked to reduced exposure to natural sunlight, disrupting circadian rhythms and serotonin levels. Factors such as geographic location, genetic predisposition, and lifestyle can contribute to the development of SAD.
Understanding these triggers is crucial for effective intervention and management, shedding light on the intricate relationship between environmental factors and mental health.
A mental health professional can provide an accurate diagnosis and recommend an appropriate treatment plan based on the individual’s needs. Here’s what you need to know:
If you or your family member is struggling with SAD, Contact The Recovery Team at (800) 817-1247 for more information and personalized mental health care.
Seasonal affective disorder (SAD) is a type of depression that occurs at a specific time of year, typically during fall and winter when daylight hours are shorter. The condition is thought to be linked to reduced sunlight exposure, affecting circadian rhythms and neurotransmitter levels.
Symptoms include low energy, irritability, social withdrawal, and changes in sleep and appetite. According to research, SAD occurs according to a summer pattern and winter pattern. There are two main types of SAD, each associated with a different season:
Fall and winter SAD, often called winter depression, is the more common form of SAD. It typically begins in late fall and extends through the winter months when daylight hours are shorter.
Individuals with fall and winter SAD may experience symptoms such as fatigue, increased need for sleep, weight gain, and feelings of sadness or hopelessness.
Less common but equally impactful, spring and summer SAD manifests as depression during the warmer months with longer days. Symptoms may include insomnia, poor appetite, weight loss, and irritability. Light sensitivity and excessive heat can contribute to the challenges faced by individuals with this form of SAD.
Several reasons contribute to the development of SAD, and understanding them can shed light on its causes.
One prominent cause of SAD is the disruption of the biological clock, also known as the circadian rhythm. The body’s internal clock regulates various physiological processes, including sleep-wake cycles and mood.
Changes in daylight duration during the fall and winter months can disturb this delicate balance, leading to mood disturbances and depressive symptoms.
Reduced exposure to sunlight is a key factor in the development of SAD. During the fall and winter, days become shorter, and individuals spend more time indoors. Sunlight exposure plays a crucial role in regulating the body’s production of serotonin, a neurotransmitter associated with mood regulation.
Insufficient sunlight can lead young people to a decrease in serotonin levels, contributing to the onset of depressive symptoms.
Serotonin, often called the “feel-good” neurotransmitter, regulates mood. Reduced exposure to natural light can lead to lower serotonin levels, which may contribute to the development of depressive symptoms associated with SAD.
According to experts, this neurotransmitter imbalance affects mood, sleep, and appetite, common areas of disturbance in individuals with SAD.
Melatonin, a hormone that regulates sleep-wake cycles, is influenced by changes in light exposure. In individuals with SAD, disruptions in melatonin levels can occur due to decreased sunlight. This can lead to disturbances in sleep patterns and contribute to the overall depressive symptoms experienced during the fall and winter months.
Several risk factors contribute to the development of SAD, including geographical location, age and gender, and family history.
According to studies, geography plays a pivotal role in the prevalence of SAD. Regions with less sunlight during fall and winter are associated with a higher disorder incidence. Inhabitants, children of northern latitudes, where daylight hours are significantly reduced in winter, are at an elevated risk of developing episodes of depression.
The limited exposure to natural sunlight disrupts circadian rhythms and melatonin production, contributing to the onset of depressive symptoms.
SAD is more prevalent in certain age groups and genders. Younger adults and adolescents are more susceptible to its effects, with symptoms often surfacing in late adolescence. Additionally, gender differences exist, with women exhibiting a higher prevalence of SAD compared to men.
The hormonal fluctuations in women, particularly during the reproductive years, may contribute to this gender disparity. The interplay of biological and environmental factors during specific life stages increases the vulnerability to winter and summer depression.
A family history of mood disorders, including SAD, significantly heightens the risk for individuals. Genetic factors contribute to the heritability of depressive disorders, and individuals with close relatives who have experienced SAD are more likely to develop the condition themselves.
Shared genetic vulnerabilities and familial environmental influences contribute to the transmission of risk across generations, emphasizing the importance of family history in understanding and identifying those at risk for forms of depression.
SAD can significantly affect mental health, leading to a range of emotional and behavioral symptoms. The seasonal nature of the disorder means that people may experience a cyclical pattern of depressive episodes, impacting their overall well-being and daily functioning.
Depression is a core component of SAD, and individuals may struggle with persistent feelings of sadness, lack of interest in activities, and low energy levels. Identifying these symptoms of changing seasons is essential for accurate diagnosis and appropriate intervention.
SAD is not limited to depressive symptoms. Anxiety can also be prevalent. People and teens may experience heightened worry, restlessness, and tension during specific seasons. The interplay between depression and anxiety in SAD underscores the complexity of the disorder.
SAD can disrupt sleep patterns, leading to insomnia or hypersomnia. Changes in the circadian rhythm, influenced by variations in natural light exposure, contribute to sleep disturbances. Consequently, individuals may experience difficulty concentrating, reduced productivity, and impaired daily functioning.
Treatment options for SAD can vary depending on the severity of symptoms, individual preferences, and specific circumstances.
Here are some main treatments for SAD:
Light bright therapy, or phototherapy, is a common and effective treatment for symptoms of Seasonal Affective Disorder (SAD). It involves exposure to a bright light miming natural sunlight, helping regulate the body’s circadian rhythms and melatonin production.
This can alleviate SAD symptoms, such as low energy and mood disturbances, especially during the darker months.
Psychotherapy, particularly cognitive-behavioral therapy(CBT), is another valuable treatment option for SAD. CBT helps patients identify and change negative thought patterns and behaviors associated with seasonal depression.
It provides coping strategies to manage symptoms and improve overall well-being.
Low sunlight exposure during winter can lead to vitamin D deficiency, potentially exacerbating SAD symptoms. While not a standalone treatment, vitamin D supplement carbohydrates may complement other interventions.
American Psychiatric Association and researchers say adequate vitamin D levels support overall health and positively impact mood and body. Consultation with a healthcare provider is crucial to determine the appropriate supplement dosage based on individual needs.
Empower your journey toward healing with The Recovery Team.
Say goodbye to winter blues and embrace a brighter tomorrow with our specialized mental health services. Our different levels of care provide personalized support for long-term healing.
In addition, our evidence-based Cognitive Behavioral Therapy (CBT) approach addresses the root causes, providing personalized strategies for lasting change.
Take the first step today. Contact us at (800) 817-1247 and let the healing begin.

Discover expert tips for repairing family relationships and fostering healthy connections with The Recovery Team.

Discover practical tips on how to set boundaries with people in this expert guide from The Recovery Team.
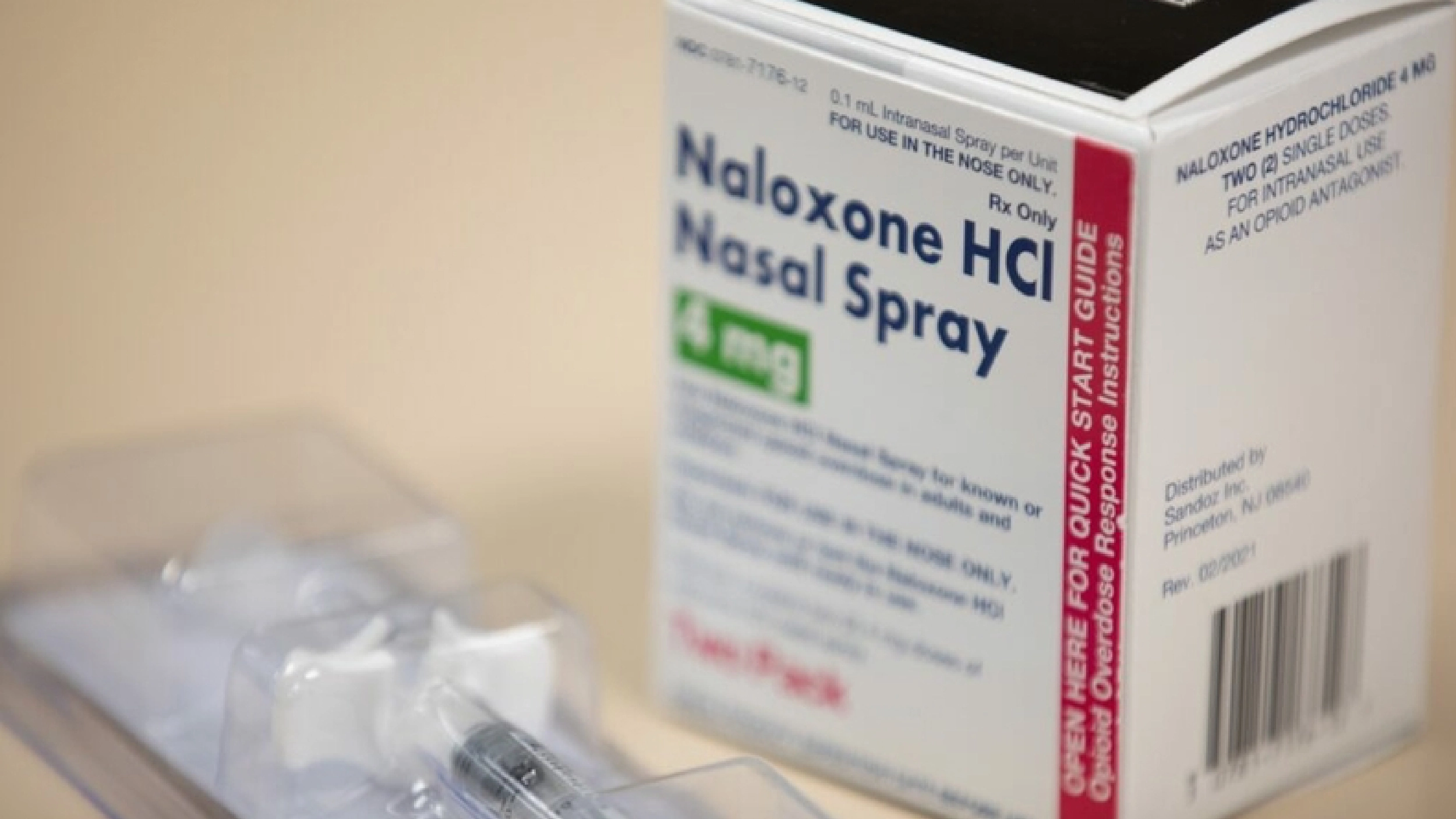
Naloxone saves lives. The Recovery Team shares how to reverse an opioid overdose with this drug.
Seasonal affective disorder (SAD) is linked to shorter days during winter, disrupting the sleep-related hormone melatonin. For some with bipolar disorder, symptoms of depression worsen in winter.
Chemical changes, lack of sunlight, and negative thoughts contribute to the winter blues. Other factors, like personal vulnerability, also play a role.
To prevent seasonal affective disorder (SAD), prioritize exposure to natural light, especially in the morning. Maintain a regular sleep schedule, exercise regularly, and consider light therapy, talk therapy, and antidepressant medications.
Consult a healthcare professional or doctor for personalized advice and treatment if symptoms persist or worsen.
Light therapy, or exposure to a bright light that mimics natural sunlight, is a common home treatment for symptoms of SAD. Spend time outdoors, maximize natural light exposure, and consider using light boxes.
Consult a mental health expert for personalized advice, medical history, and potential additional interventions.